In 2025, there were 2267 cases of measles in the United States, and 70% of those were in children. 11% were hospitalized. There were 3 deaths from measles. These are the first measles-related deaths in the United States in a decade. 2026 is trending to be worse, with 588 cases by the end of January. (In 2024, there were only 285 cases in the entire year.)
So it’s time for an update on measles: what is it, how contagious is it, and how to prevent the spread (hint: the measles vaccine substantially reduces your risk.)

What is Measles?
Measles symptoms appear 7 to 14 days after contact with the virus. Measles typically begins with: High fever (may spike to more than 104°), cough, runny nose, red, watery eyes.
2 – 3 days after symptoms begin, white spots in the mouth may develop.
3 – 5 days after symptoms begin, the measles rash appears: beginning as flat red spots that appear on the face at the hairline, then spread downward to the neck, trunk, arms, legs and feet. Small raised bumps may appear on top of the flat red spots. The spots may join together as they spread. The fever may spike to more than 104.
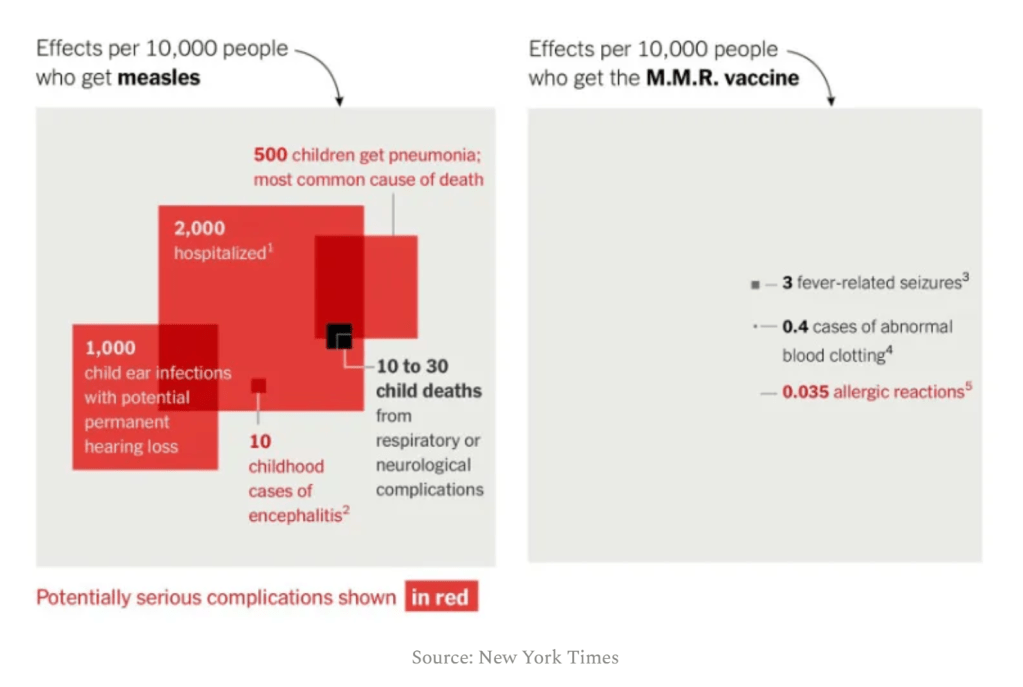
Measles can cause serious problems, including ear infections (1 in 10 people with measles), pneumonia (1 in 20), and encephalitis (1 in 1000) which can cause permanent brain damage. About 1 in 10 people who get measles in the U.S. will be hospitalized. (For kids under 5, there’s a 1 in 5 chance of hospitalization.) Even after recovery, it has a long-term effect on your immune system, making you more vulnerable to other diseases.
You may hear some people say “measles can be treated with vitamin A” as if to imply that it is a minor and easily treatable illness where you pop a few vitamins and it’s resolved. Although vitamin A does have benefits in reducing mortality in children who already have measles (especially in countries with high levels of vitamin A deficiency), preventing a child from getting measles in the first place is a far better way to reduce measles mortality. Vitamin A does not protect someone from infection with measles (it’s not preventative), and if a child does have measles, parents should not self-treat with vitamin A without consulting a physician.
Is measles deadly?
No, not for most people. (For example, I learned today from looking at my health records that I had measles as a baby, in 1967.) However, for every 10,000 people who get measles, 10 to 30 children will die.
You may hear some people say things like “a lot more people die of flu each year than measles”, with the implication that measles is not that risky. No. The reason is that since measles vaccines became available, measles had become a fairly rare disease. In 2023, there were 59 cases of measles in the US and 40 million flu-related illnesses, so of course there were more flu deaths.
Before the measles vaccine existed, there were 3 to 4 million cases per year in the US and 400-500 people died. After the vaccine became available, rates plummeted. Many pediatricians across the US have never actually seen a case of measles. The fact that the rates of infection, and thus deaths, had dropped so far should be seen as a huge success for modern medicine.
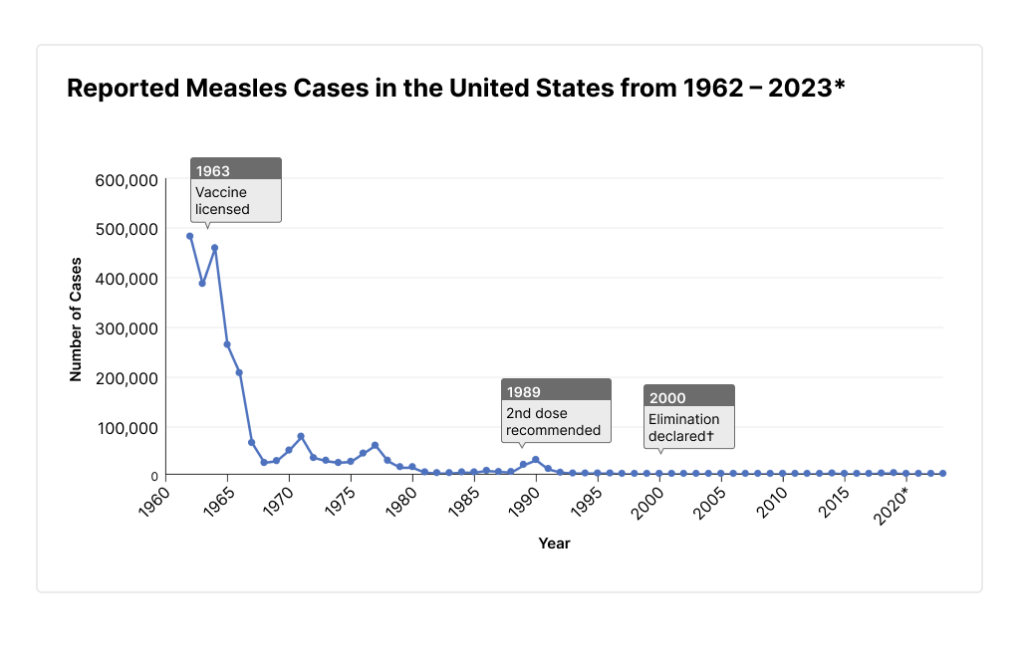
Unfortunately, due to widespread misinformation about MMR vaccines, and the fact that parents who have never seen measles mistakenly believe it to be mostly harmless, vaccination rates are dropping, and we will start seeing more measles cases each year.
How Contagious is Measles?
For people who are not vaccinated / immune, it is the most contagious virus on Earth.
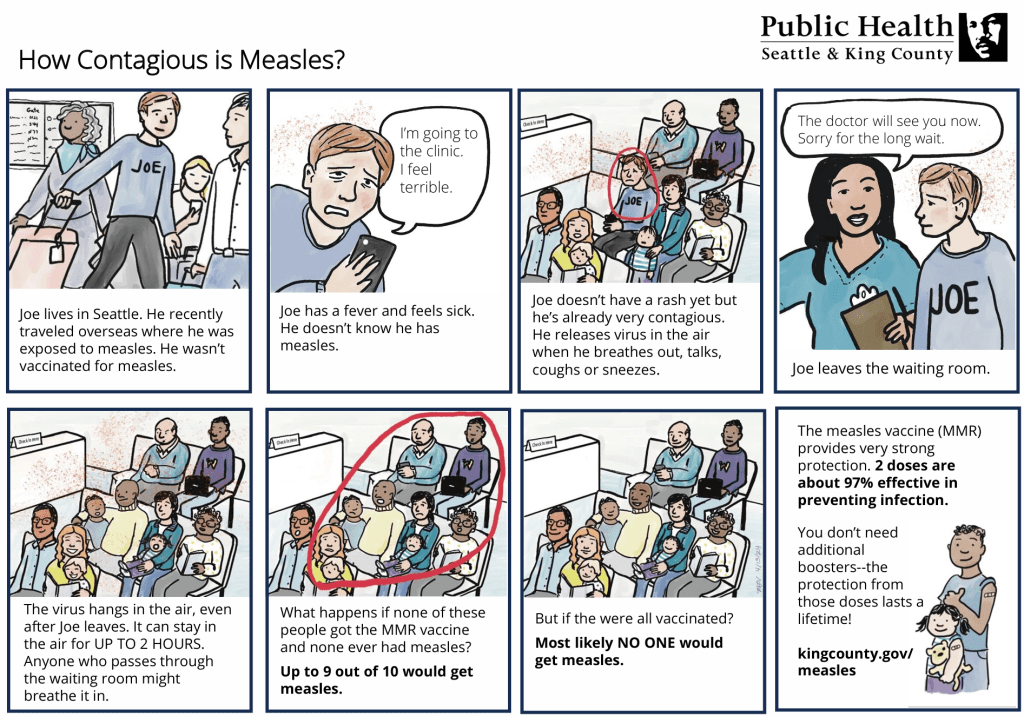
When someone has the measles, they may develop fever and other symptoms before the characteristic rash appears. (They may be infectious for 4 days before the rash appears.) So they may not realize they have measles, and may be out in public – in school, restaurants, shops, buses or medical clinics. If they cough or sneeze, they produce infected droplets, that can remain active in the air or on surfaces for up to two hours. If people who are not vaccinated / immune are exposed to the contaminated air / surfaces, the chance they will develop measles is 9 out of 10.
On average, every person with measles will spread it to 12 – 18 unvaccinated people.
If you or your child has been exposed to measles, contact your doctor.
Protecting against Measles
For those who are fully vaccinated, their chance of getting infected after an exposure is about 2 in 100 (vs. 90 out of 100 for those who aren’t vaccinated.) And, even if a vaccinated person does get an infection, it will be much milder, with many fewer complications and they will be less infectious than in someone who is not vaccinated.
The more people in a community who are vaccinated, the lower the risk of an outbreak. If at least 95% are vaccinated, that’s considered herd immunity or community immunity and that reduces the risk of the spread in that community.
In King County, Washington, 97% of our 6th/7th graders are vaccinated against measles, but only 92% of kindergarteners are, and only 87% of 2 year olds. (And, 0% of babies under 6 months old since they are not yet old enough for the vaccine, so are at the highest risk of infection.)
It is recommended that children receive a dose of the MMR vaccine (which includes measles) at 12 to 15 months. [If your community is having an outbreak (3 or more related cases) or you are traveling internationally, they can receive that dose as early as 6 months. Learn more about protecting infants.] That provides 93% protection against infection. They should have the second dose at 4 – 6 years, which brings them up to the 97% protection. If your child is not vaccinated, you can get them vaccinated at any time. Learn more. You can also get vaccinated yourself if you are not – check for contraindications (e.g. you can’t get the MMR vaccine while pregnant.)
If you have already been exposed to the measles virus, getting a vaccine shot within 72 hours of exposure (or an immunoglobulin medicine within 6 days of exposure) will help reduce the chance of infection / the severity of the illness.
Vaccination is the single best way to reduce risk of infection. You can also reduce risk with all the usual things: handwashing, hand sanitizer, and limit exposure to people who show signs of illness.
Am I Immune?
You are presumed to be immune (and thus don’t need a vaccine) if you have:
- written documentation of your past vaccines (children age 1 – 3 should have one dose, age 4 – 18 two doses, for most adults one dose is enough but healthcare providers and international travelers should have two)
- a lab test that shows immunity
- laboratory confirmation of disease
- were born before 1957 (it’s assumed that most people born before 1957 had the illness at some point)
If you received a LIVE measles vaccine in the 1960’s you do not need to be revaccinated. But, if you received an inactivated measles vaccine between 1963 and 1967, it was not effective and you should be revaccinated. If you’re unsure: You can ask your doctor for a blood test to check for immunity, or just get the vaccine. The MMR vaccine is safe. There’s no harm in getting another dose.
Is the vaccine safe? What are the side effects?
Common side effects are: Soreness, redness, or swelling where the vaccine was given, fever, mild rash, and temporary pain and stiffness in the joints. More serious side effects, such as a high fever or a febrile seizure are rare.
The MMR vaccine does not cause autism.
If your child is due for any shot, check out these tips for how to make shots less stressful.
Note: I am an educator, not a health care professional. For professional, evidence-based info on any of the topics above, please click on the links above. Or go to https://www.healthychildren.org/english/health-issues/vaccine-preventable-diseases/Pages/Measles.aspx, https://www.aap.org/en/patient-care/measles/ or https://emilysmith.substack.com/p/measles-updates